An explosion of gunfire fills your ears as you lay on your back, blood seeping out from the bullet wounds in your shoulder and lower abdomen. You are barely coherent and so weak from blood loss and pain that you can’t move. Your weapons were powerless against the brutal and sudden attack from the enemy. Two of your fellow soldiers are dead beside you; you watched them fight like lions and die by your side. You are in shock, surrounded by death, and your life is a hairsbreadth from slipping away. Even though adrenaline is pumping through your veins, you lose consciousness.
When you wake again, the doctors have pieced your broken body back together…
but you are not the same person.
PTSD. Post-Traumatic Stress Disorder. What comes to mind when you hear those words? You probably picture something very similar to the war experience I described above.
According to the U.S Department of Federal Affairs, approximately 10-20% of war veterans have PTSD.
War veterans are respected, admired, and people generally understand why they struggle with post-traumatic stress.
At this point, you may be thinking: “Aspen, why the heck are we talking about soldiers of war and not cancer patients?”
Well, you see, like the good little writer I am, I am setting us up for an awesome (and incredibly important) analogy.
You see, cancer patients fight on their own battlefield. And it’s time people understood this.
While it is commonly known that soldiers of war can develop PTSD, it is not known that cancer patients are also at high risk for developing that same disorder.
My goal here in today’s post is to briefly discuss PTSD and (more importantly) compare soldiers of war with cancer patients.
What Is PTSD? What causes it? Excellent questions!
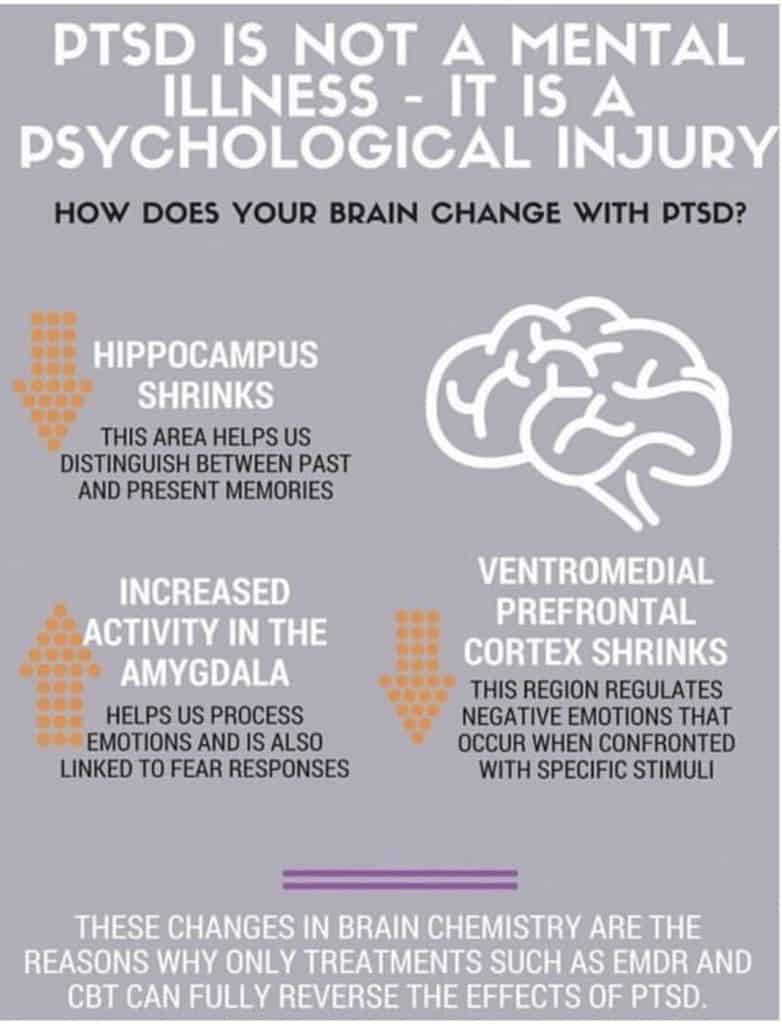
Post-traumatic stress disorder (PTSD) is a mental health condition that’s triggered by a terrifying event — either experiencing it or witnessing it.
Typically, it is caused by PTSD commonly develops in response to traumatic or life-threatening experiences such as war, sexual assault, accidents, or natural disasters. These situations all involve traumatic circumstances, severe levels of stress, and a direct threat to a person’s life or bodily integrity.
To summarize, events that involve traumatic events such as death, the threat of death, actual or threatened violence, or serious injury can all lead to the development of PTSD.
Symptoms of post-traumatic stress disorder may include flashbacks, nightmares and severe anxiety, depression, anger, panic, as well as uncontrollable thoughts about the event.
Yeah, I know. It sounds pretty bad, right?
But wait! This symptoms list continues:
Avoiding places, events, people, or things that bring back bad memories, strong feelings of guilt, hopelessness, or shame, trouble sleeping or concentrating, continuous feelings of fear or anger, loss of interest in activities and relationships that used to be enjoyable, self-destructive behavior including drug or alcohol abuse or self-harm, and suicidal thoughts (just to top it all off).
Now that we have a general understanding of what PTSD is and recognize that severe stress and trauma play a large role in its development, I want to draw some very important parallels.
Soldiers of war commonly develop PTSD because they face ongoing threats to their life, experience intense or long-lasting physical pain, or witness other soldiers deaths. As I mentioned above, this is common knowledge. But now I want to share a new perspective.



Where soldiers worry about being killed every day, cancer patients worry about their own survival for months or years while they undergo chemotherapy treatment. They wonder if their cancer will win out in the end, fear dying on the operating table during an emergency surgery when they have no blood counts, and they are at high risk to contract deadly infections with their non-existent immune systems. This is if a patient’s cancer is even survivable at all.
Where soldiers experience discomfort and pain due to injuries and undesirable living conditions, cancer patients undergo surgeries, amputations, and spinal taps. They endure hospital stays where they are poked with needles, woken up repeatedly every night, and hooked up with tubes to IV poles. They are injected with chemicals so toxic that their hair falls out— chemicals that cause pain, nausea, neuropathy, inability to sleep, organ damage, skin rashes, mouth sores, and an endless list of other side effects.



Where soldiers watch their squad members die, cancer patients witness other cancer patients in the treatment facilities and hospitals succumb to their cancer.
This may very well be the most important analogy I ever give on this blog. This is a perspective I think everyone should understand.
For some reason, most of society considers soldiers of war to be the only respectable candidates for PTSD. But post-traumatic stress does not discriminate between battlefields. This kind of mental trauma occurs when people are confronted with certain traumatic stimuli that BOTH soldiers and cancer patients encounter.
Two enemies. Two different battlefields. But a common tormentor of post-traumatic stress
AND THIS IS NOT A DISTANT PROBLEM!
Data by the National Cancer Institute shows that approximately 38.4% of men and women will be diagnosed with cancer at some point during their lifetimes.
This is nearly 1 out of 2 people.
New research is showing that we are only beginning to scratch the surface in the study of cancer patients and PTSD and that it’s possible the two have a BIGGER correlation than is currently known.
I recently gave a speech about this topic in my public speaking class at the University of Colorado Boulder. I won the award for the best speech in the class.
Near the end of my presentation, I said this: “Now that we have drawn undeniable parallels between soldiers of war and cancer patients, I hope that you all can leave here today with a new frame of reference through which you can view cancer patients and survivors.”
And I accomplished my goal!
I didn’t even need to go into the science of post-traumatic stress to help them understand. (And, never fear, I will be going into all that awesome neuro-science stuff at a later time!)
All I had to do was draw obvious connections between something that people generally accepted and something foreign.
I walked out of that room after my speech knowing I’d convinced my audience that cancer patients are at high risk for developing PTSD.
But this is not just something that cancer-free people need to hear.
The fact that cancer patients are at high risk for PTSD is something everyone battling cancer should know.
Many of the cancer patients I encounter struggle with a lot of symptoms of PTSD without recognizing why or even considering that they may be suffering from a degree of Post-Traumatic Stress. And you can’t treat what you don’t understand.
Not every cancer patient will struggle with PTSD, but the traumatic and life-threatening experiences that a majority of cancer patients have put them and survivors at really high risk for this kind of mental trauma.

(Yes, this is me!)
I want to share with you how I concluded that speech I gave:
“I hope this topic feels a bit personal because it is. Most likely, only a few of you walked into this room today knowing someone with cancer, but all of you will leave knowing that you have been within ten feet of a cancer survivor. I am a leukemia survivor.
And I fought my own battle during the three years of intensive chemotherapy where I faced pain and trauma, underwent life-threatening emergency surgeries, watched friends succumb to their cancer, lived in hospitals, and spent every single day knowing that I was a hairsbreadth from death.
And when my chemotherapy finally ended, I dealt with PTSD for years. And I was not granted the understanding that soldiers are given.”
(BTW, if you ever want to shoot yourself in the foot socially, this is a surefire way to do it)
What I didn’t tell my fellow students is that I STILL struggle with PTSD. They didn’t need to know. I wasn’t giving that speech to make them think about me. I wanted them to think about cancer patients in a new light. But I can tell you all here on my blog that I do still struggle a lot.
I have been aware of my own PTSD for a long time, and that alone has helped me learn to manage it and learn to challenge those feelings when they come up. But sometimes, it just completely sweeps me off my feet.
I’m talking full-on mental breakdowns. Sometimes, I am screaming, throwing things, and hitting myself. Other times it comes in the form of having a panic attack that reduces me to crying on the floor in the fetal position, my hands clutching my head to my chest and feeling like I can’t move or breathe.
There are times when I get triggered, and everything just goes to shit. My family can attest to this.
And I feel so completely powerless to stop any of it…
There are times when it physically feels like I can’t. And the things I say and do when I am struggling with PTSD are so unlike me. Those of you who know me personally know that anger and violence are the farthest things from my personality.
To give you an example:
It’s like how you can take a perfectly sweet and loving dog with a history of horrible physical abuse. As soon as you raise your hand the wrong way, you can reduce this sweet dog to a ferocious beast who tries to attack you OR you can turn it into a shaking, cowering creature that is too terrified to move.
Ever since I was diagnosed with leukemia, I have felt like a traumatized animal more times than I can count. I still feel this way in my present life.
And struggling with PTSD has been one of the most difficult and impactful challenges I have been facing for the last five years of my life.
In my next post, I intend to go in-depth about my experiences with PTSD. I will explain some of the most traumatic events that contributed to its development, describe what triggers me now, and give the cringe-worthy details of how my PTSD manifests itself. It will be a good read!
(I also encourage all of you to share this post with anyone you know that might benefit from hearing my soldier-cancer patient analogy!)
Latest posts by Aspen Heidekrueger (see all)
- How My Chemo Treatment Led To An Eating Disorder (PART 2) - November 16, 2020
- How My Chemo Treatment Led To An Eating Disorder - November 8, 2020
- Another Encouraging Word for Cancer Survivors (And Everyone Else) - October 25, 2020

This really made me think
Let’s hope it makes everyone else think too. More people need to be aware of this.
Thanks for that brutally honest picture of what you struggle with. It makes me so angry that you have to experience the effects of a disease that very nearly took your life, along with the ongoing effects of the very treatment efforts that saved your life. I so wish our country could spend just 10% of what we spend blowing up remote portions of our world and direct the funds to research into cancer and it’s long term effects, including treatment for PTSD!
Being left to deal with all the trauma and long-term side effects of chemotherapy is itself an unfortunate side effect of surviving cancer. There are so few resources for cancer survivors to use in their recovery from PTSD. No one funds anything like that, and 90% of people don’t even know that cancer patients struggle with PTSD. All I can do for now is just try to spread the word about the challenges cancer patients face and offer my own personal support. Thanks for your comment!
Thank you for sharing all this hard stuff Aspen. It helps me to understand more of where you are coming from. It also makes me very sad. So a lot of time and money went into treating cancer, now we need to spend just as much time and energy in treating the after affects of the treatment. And where does the money come from to treat the after affects?
I love to use analogies in my writing because there is a huge gap to be bridged between cancer patients and those who have never had cancer. It is so hard for people to understand exactly what cancer patients go through, but it is really important that more people are made aware. And I agree, there is too little energy, time, or money put into helping cancer patients recover. Being left on your own to deal with so many physical and emotional problems is an unfortunate side effect of being a cancer survivor.
Aspen, this is…beautiful, heartbreaking, inspiring, painful and encouraging all at the same time. You are an amazing writer, and the fact that you’re using your skill in writing to support, encourage and relate to others who have experienced or are experiencing cancer is…miraculous. I hope this blog, and writing all this out helps you heal and helps you reflect and release all of it, because it’s all so good and hard and…real. I admire your authenticity and vulnerability with all this hard stuff, and I admire your heart and your desire to inspire, uplift and encourage those who have been… Read more »
Caleb, Thank you so much!! Your kind words and compliments just make my heart happy. This blog and everything I write on it is so important to me. It is a HUGE part of my own healing process. I have such a big desire to have everything I have been through recorded. I want my experiences to be outside of my head. There is so much that I don’t want to forget. Another huge reason is that I want people to know how much I have been through. I want the world to see how hard I have fought so… Read more »